Gestational Hypertension, What You Need to Know
Gestational hypertension is also referred to as pregnancy induced hypertension (PIH). It is for this reason you will find the two often used interchangeably.

Gestational high blood pressure is the most frequent cause of hypertension in women who are pregnant. On the whole it affects between 6 to 8% of pregnant women. Furthermore, it complicates 6 to 10% of those pregnancies (see complications later below).
Gestational high blood pressure risks can be extremely severe to the extent of growth retardation also known as intrauterine growth restriction (IUGR), prematurity and intrauterine death also refereed to as fetal demise or stillbirth.
Accordingly, in order to consider what could be done to avoid, manage or treat gestational hypertension, it's necessary to define it...and here is how...
Pregnancy Induced Hypertension Definition
According to a review article shared in the 2015 edition of the journal, Hormones (2015, 14(2):211-223), the definition of pregnancy induced hypertension is centered around specific blood pressure measurements.
While in simplified terms gestational hypertension is high blood pressure that occurs in pregnancy, the clinical definition used by physicians once pregnancy is confirmed specifies blood pressure vales consistent with gestational high blood pressure as systolic blood pressure (top number) greater than 140 mm Hg and diastolic blood pressure (bottom number) greater than 90 mm Hg.
By the same token physicians further classify pregnancy induced hypertension as mild, moderate and severe, were mild is systolic blood pressure (SBP) between 140-149 mm Hg and diastolic blood pressure (DBP) between 90-99 mm Hg.
Similarly, moderate gestational high blood pressure is SBP of between 150 to 159 mm Hg and DBP is between 100 to 109 mm Hg.
The definition of pregnancy induced hypertension further classifies severe gestational hypertension as SBP equal to or greater than 160 mm Hg and DBP of equal to or greater than 110 mm Hg.
Here are the clinical parameters which define pregnancy induced hypertension summarized in table form:-
|
Systolic Blood Pressure |
Diastolic Blood Pressure | |
|
Pregnancy Induced Hypertension (PIH) |
>140 mm Hg |
>90 mm Hg |
|
Mild PIH |
140-149 mm Hg |
90-99 mm Hg |
|
Moderate PIH |
150-159 mm Hg |
100-109 mm Hg |
|
Severe PIH |
≥160 mm Hg |
≥110 mm Hg |
Pregnancy Induced Hypertension Causes and Risk Factors
To the relief of many an expectant mother, the advancement of science over time has done a great deal in shedding light on the causes of high blood pressure during pregnancy.
It is important to realize that pregnancy is of itself a physiological change that happens to the body. This change induces increased cardiac or heart output and an increase in blood volume, for example. These changes take place with different effects over the duration of the pregnancy.
In normal pregnancy, blood pressure is reduced during the first trimester, continues to fall to its lowest point at mid-way of pregnancy before returning to pre-pregnancy levels during the course of the third trimester.
The most compelling evidence from studies implicates the placenta in gestational hypertension as it interacts with a number of systems including the cardiovascular system.
In sustaining this observation of the role of the placenta in causing pregnancy induced hypertension, a June 2001 review published in the American Journal of Hypertension (2001 Jun;14(6 Pt 2):178S-185S) noted that a yet to be fully explained occurrence related to gestational hypertension causes reduced placental perfusion.
Placenta perfusion refers to the exchange of oxygen, nutrients, blood and other fluids, among a host of biochemical activity, between the mother and the baby while in the womb.
Compromised perfusion, researchers suggest, results in the general dysfunction of the mother's vascular endothelium. Vascular endothelium refers to cells lining the interior of blood vessels along the entire circulatory system. Endothelium is critical in blood pressure regulation as it influences the relaxation or constriction of blood vessels a major factor in hypertension.
As shown in studies involving both animals, such as sheep, dogs and rabbits, and also humans, blood flow restriction related to reduced placenta perfusion results in elevated blood pressure.
Furthermore, women with gestational hypertension fail to respond in a similar fashion as women with normal pregnancy to pregnancy related increased blood output and blood volume.
On the contrary, instead of decreased blood flow resistance in response to an estimated 40 to 50% increase in cardiac output and blood volume related to pregnancy, peripheral resistance is actually increased in women with pregnancy induced hypertension. Peripheral resistance refers to the constriction and dilation of blood vessels to increase or decrease blood pressure.
Poor Nutrition as a Cause of Pregnancy Induced Hypertension
The role of nutrition as both a risk factor and a potential cause of pregnancy induced hypertension has also received some worthy attention.
A study published in the May 2013 journal, Hypertension in Pregnancy (2013 May;32(2):146-56), put forward some evidence backing the idea that nutrition does play a role in the development of gestational hypertension. The study seemed to suggest that poor nutrition caused pregnancy induced hypertension.
Carried out at Shahid Akbarabadi Hospital in Tehran, Iran, the study involved 263 women 113 with pregnancy induced hypertension and another 150 healthy pregnant women without gestational hypertension.
The study which focused on the diet of the women revealed that women who took higher intakes of energy who had a diet with monounsaturated fatty acids and polyunsaturated fatty acids had a greater risk of developing pregnancy induced hypertension. This was also the case in women who took lower intakes of vitamin C, of potassium and magnesium.
These dietary foods had a positive correlation with the risk of developing pregnancy induced hypertension.
Elsewhere on this website, we have also extensively looked at the association between potassium and high blood pressure in a general sense which also applies to pregnant women.
All things considered, the Tehran study only adds to other such already existing evidence that diet is critical to gestational hypertension and high blood pressure in general.
Other such evidence include a meta-analysis report of several studies published in the September 2014 issue of the journal BMC Medicine (2014; 12: 157) which placed an association between higher total energy, lower magnesium and calcium intake measured during pregnancy with hypertensive disorders of pregnancy (HDP).
Who Is at Risk of Pregnancy Induced Hypertension?
It's a natural inclination to want to know how much one could possibly be predisposed to gestational hypertension particularly so for first time parents. The following are some indicators of who could be at risk of pregnancy induced hypertension.

Source: Human Resources Online
- Being older than 40 years of age
- Being Black or Hispanic
- Antiphospholipid syndrome (APS), sometimes known as Hughes syndrome and also associated with blood clots
- Relative risk of preeclampsia
- Previous preeclampsia
- Insulin-dependent diabetes
- Multiple pregnancy (women carrying multiples)
- Nulliparity (not having carried pregnancy or given birth before)
- Family history of preeclampsia
- Obesity
- Weight gain during pregnancy
- Low mother Vitamin D
- Preexisting hypertension
Pregnancy Induced Hypertension Complications
Pregnancy complications caused by gestational hypertension may occur early or late in pregnancy affecting both mother and baby. Nevertheless, studies observe that pregnancy induced hypertension complications occur more frequently during the early-onset period which is before gestational week 32.
For better clarity, we have categorized potential complications as follows;

Mother Complications
On a long term basis beyond the pregnancy, gestational hypertension increases the risk of chronic hypertension and kidney disease later in life.
A 2013 study published in PLoS Medicine (2013;10(4):e1001425) presented evidence that, compared to women without hypertension, women with pregnancy induced hypertension ran a 2-fold higher risk of developing diabetes some 16.5 years later after pregnancy.
Not only so, another complication arising from pregnancy induced hypertension in women is the rapture of red blood cells known as haemolysis. This results in hemoglobin being released into blood plasma potentially causing things to go down hill from thereon.
HELLP may also occur due to high blood pressure in pregnancy. HELLP syndrome is a life threatening combination of hypertension complications that includes hemolysis (H), elevated liver enzymes (EL) and low platelet count which stops blood from clotting (LP). HELLP occurs in later stages of pregnancy or in some cases even after pregnancy.
Similarly, the dysfunction of the central nervous system may also occur due to elevated blood pressure during pregnancy. This may go as far as affecting the structure and the functioning of the brain and the spinal cord.
One of the more serious pregnancy induced complications is placental abruption. This is life threatening to both the mother and baby and follows a partial or complete separation of the placenta from the uterus while the baby is still in the womb. This severs oxygen, nutrients and blood supply.
Hepatocellular injury which relates to damage to the liver is lingering potential result of gestational hypertension complications. Thrombocytopenia is an additional poor out come of elevated blood pressure in pregnancy. It relates to lower than normal counts of platelets in the blood. Symptoms of it include prolonged bleeding and blood in urine or stools.
The following is a summary of complications occurring to the mother.
- Long term/Later life hypertension
- Diabetes
- Cardiovascular disease (CVD)
- Haemolysis (red blood cell rapture)
- HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count)
- Nervous system dysfunction
- Placenta abruption
- Hepatocellular injury (liver injury)
- Thrombocytopenia (low blood platelet count)
- Acute disseminated intravascular coagulation (DIC) (formation of blood clots through out the body's small blood vessels)
- Oliguria or hypouresis (reduced urination)
- Pulmonary edema (excess fluid in lungs with potential for respiratory failure)
- Intracerebral hemorrhage (ICH) (bleeding in the brain)
- Cerebrovascular event (stroke)
Baby Complications
Similarly, there are gestational hypertension complications that affect the born and unborn baby.
In the first place is intrauterine growth restriction (IUGR), a pregnancy complication related to gestational hypertension that occurs when the weight of the baby is below what is expected for gestational age.
Gestational age itself refers to how far along the pregnancy is in its timeline.
IUGR is determined by an ultrasound and while caused many things its most leading causes are malnutrition and a low supply of oxygen factors that are also known to result from the mother's high blood pressure.
Together with IUGR, another pregnancy induced complication that affects the offspring is low birth weight neonate or new born. This is a new born birthed weighing about 2.5 kgs compared to the average desired of 8 pounds or 3.6 kgs.
In addition, high blood pressure may also induce birth of the baby before 37 weeks which is refereed to as preterm birth or premature birth.
In the longer term, babies born to gestational hypertensive mothers have a higher risk of developing higher blood pressure in childhood and as mature adults. Such individuals have also been shown to have a double risk of stroke and mental disorders later in life.
Here is summary of pregnancy induced complications in babies;
- Intrauterine growth restriction (IUGR)
- Preterm birth or premature birth.
- Hypertension later in life
- High risk of stroke later in life
- Cognitive challenges in life
- Possible Mental disorders later in life
- Impaired lipid profile in life ( a risk factor for sexual dysfunction in females among other problems)

Gestational Hypertension Treatment
The definitive treatment of gestational hypertension, researchers are agreed, is delivery.
However, were gestational age is below 32 weeks the question remains, what can be done. Treatment of gestational hypertension is a multi-faced approach.
Beyond the initial screening for pregnancy induced hypertension, target organ damage is also assessed in addition to any underlying causes of the high blood pressure which may confirm secondary hypertension.
Frequent visits to see a doctor or healthcare provider along with scheduling timely delivery are important aspects of managing pregnancy induced hypertension. Delivery may be delayed to allow full maturity of the baby particularly the respiratory system to reduce risk to the baby at birth. Counseling to assist the pregnant mother make informed decisions is also critical.
While lifestyle changes such as weight loss and reduced salt intake have been shown to be of benefit in the general population which is hypertensive, the same cannot be said of pregnant women.
In addition, although salt restriction is almost rule of thumb in hypertensive people, due to volume contraction in pregnancy dietary salt reduction is not regularly recommended even in hypertensive pregnancy women.
Volume contraction refers to a reduction in body fluids including in blood vessels which has a play on blood pressure itself.
A February 2003 report in the British Journal of Sports Medicine (2003 Feb; 37(1): 6–12), did not show any evidence of benefit from weight loss towards high blood pressure in pregnancy. There is still limited research into whether these types of lifestyle changes are useful in pregnancy.
However, weight gain should be avoided prior to pregnancy according to the Institute of Medicine.
In this regard, guidelines by the Institute state that women who are overweight before becoming pregnant should only gain between 15 and 25 lbs during pregnancy. This is in contrast to those of normal weight prior to pregnancy who could gain 25 to 35 lbs.
A regularly applied gestational hypertension treatment option is bed rest. A 2008 study evaluated the effects of restricted activity in pregnancy.
It was published in the journal Hypertension in Pregnancy (2008;27(2):197-205) and concluded that when strictly adhered to, bed rest is very effective in prevention of pregnancy induced hypertension.
Not only that, bed rest was also effective in treating poor growth of the baby in the womb (intrauterine growth restriction). The research conclusions were drawn from data on over 600 women who were prescribed bed rest in hospital.
Gestational Hypertension Treatment Using High Blood Pressure Medications
High blood pressure medications have been used to treat pregnancy induced hypertension. The use of pharmaceutical drugs to treat gestational high blood pressure has been shown to stop the progression of high blood pressure in pregnancy to severe hypertension as well as stopping mother related complications such as heart failure and stoke.
The drugs have also been used to help with maturity of the baby in the baby by increasing its gestational age.
According to the journal Hormones (2015 Apr-Jun;14(2):211-23), how gestational hypertension is treated depends on factors such as blood pressure levels, gestational age, presence of symptoms and any associated risk factors.
For instance, in cases were SBP is between 140-149 mm Hg or DBP is between 90-99 mm Hg, treatment should be limited to non-drug therapy.
Furthermore, antihypertensive treatment is recommended in cases of gestational hypertension were blood pressure values are greater than 140/90 mm Hg.
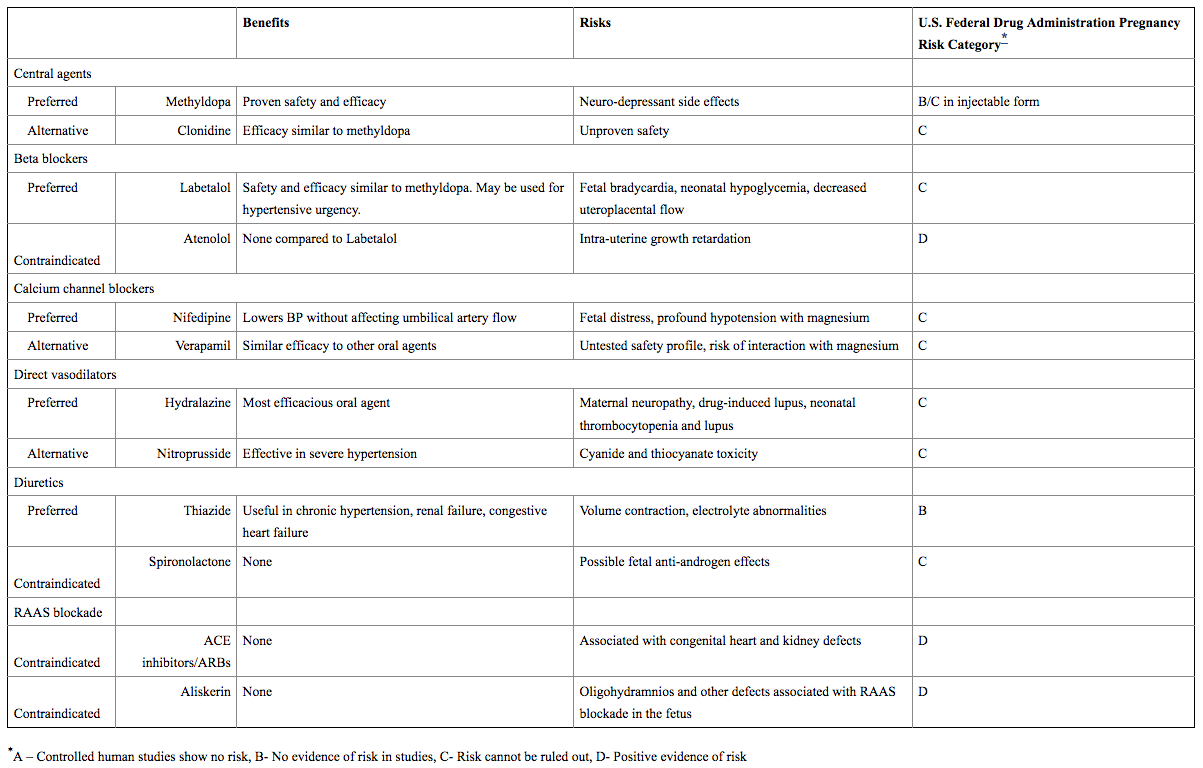
Concerning which drugs to use, diuretics have been shown to be beneficial. In contrast drugs such as ACE inhibitors have shown no benefits and have been linked to congenital heart and kidney defects and therefore concluded to have positive evidence of risk and therefore contraindicated.
The table below details the available drugs and their respective benefits and risks in treating gestational hypertension.
Medication choices for pharmacologic treatment of hypertension in pregnancy
Source: Advances in Chronic Kidney Disease
[Last updated: 25 October 2017]

|
|
Alcohol and Blood Pressure |
Return to Hypertension Causes from Gestational Hypertension
Return to Hypertension Home Page from Gestational Hypertension
Disclaimer
Information contained on this website is not meant to replace your doctor's advice.
(c) All Rights Reserved. 2010-2018
Supplements have been shown to help in treating gestational hypertension in pregnant women. Here are the three foremost supplements used in treating pregnancy induced hypertension and their recommended daily doses.

Take 300 mg daily. This amount of magnesium supplementation has been shown in studies to reduce the severity of gestational high blood pressure. Relying on dietary intake alone is often not enough to meet the daily recommended levels. This is were supplementation is recommended.

Take 1200 to 1500 mg daily. We have also written about the benefits of calcium in treating general hypertension. The National Institutes of Health (NIH) recommends pregnant women take 1200 to 1500 mg daily of calcium supplements. No side effects have been identified for both mother and baby.

Take 20 mg daily. A double-blind study done on Hispanic pregnant women concluded that zinc was effective in reducing the effects of gestational high blood pressure in the women.