Prehypertension Fully Explained
Prehypertension also known as pre-high blood pressure or in short pre-HTN, has not always been known as such. As you shall shortly see, it's a relatively new term in hypertension science.

Until 2003 following a change in guidelines by the Joint National Committee (JNC) in its seventh guideline, which is also known as JNC-7, people suffering from pre-HTN were classified as normotensive. Normotensive refers to individuals with normal blood pressure readings.
Because for many years pre-HTN individuals were erroneously considered normotensive and therefore healthy, it allowed such individuals to possibly progress to hypertension later in life without the opportunity for treatment. This undoubtedly increased their risk of cardiovascular complications. Complications that come to mind include stroke and heart attack.
For the purpose of clarity to our readers, the Joint National Committee (JNC) is an initiative of the The National Heart, Lung, and Blood Institute (NHLBI) in the United States. It has world wide renown beginning in the mid-70s of assembling experts "to oversee the publication of reports for the prevention, detection, evaluation, and treatment of high blood pressure (BP)".
Pretty much everyone in the hypertension research community has been guided in one way or the other by JNC reports.
The first report by the JNC was in 1976 with new reports produced every 4 to 6 years. The JNC-7 report was in 2003 in which a new class of hypertension, pre-HTN, was given birth. A brand new clear cut definition of prehypertension was proffered.
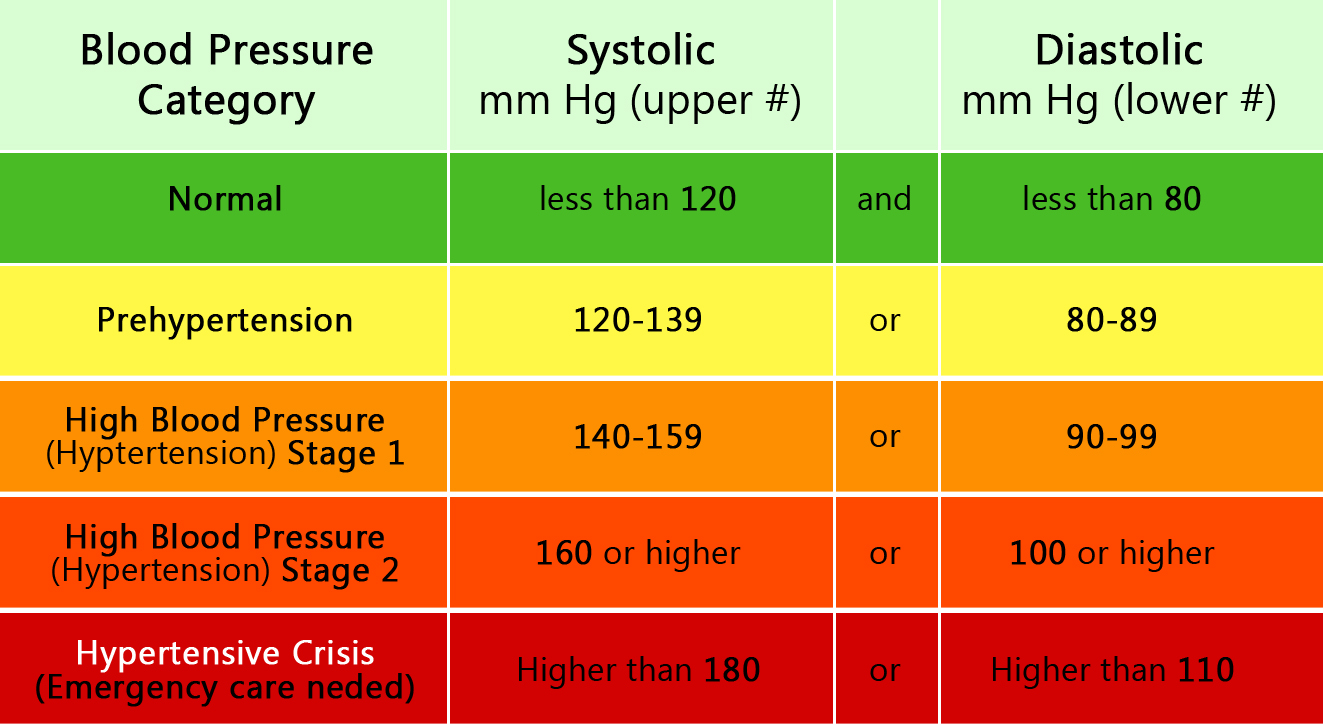
Prehypertension Definition and Readings
Since JNC-7, a new definition of blood pressure readings which were
higher than normal but not exactly hypertensive was found. This
classified individuals within a certain blood pressure reading range as
suffering from prehypertension.
Therefore, pre-high blood pessure is a situation were one is not hypertensive nor are they considered as having normal blood pressure
According to JNC-7, the definition of prehypertension is when systolic blood pressure (top number) readings are anywhere between 120 and 139 mm Hg or diastolic blood pressure readings are between 80 and 89 mm Hg.
Notably, pre-HTN readings are just above the optimal level blood pressure readings which are more than 120 mm Hg over 80 mm Hg and less than 140 mm Hg over 90 mm Hg (120/80-140/90).
The following infographic illustrates the relationship between normal blood pressure, other hypertension sub-tpyes and pre-high blood pressure.
The reasons why it was critical to establish a clinical prehypertension definition of blood pressure were motivated by previous studies which showed that hypertension was more likely to occur in people who had pre-high blood pressure. Furthermore, studies also presented convincing evidence that prehypertensive people were at higher risk of developing cardiovascular diseases (CVDs)
In support of this understanding, a 2004 study published in the Archives of Internal Medicine (2004 Oct 25;164(19):2119-24), showed that the elimination of pre-HTN reduced premature deaths, hopitalizations and nursing home admissions.
Surprisingly, the investigation found that pre-high blood pressure was responsible for 3.4% of hospitalizations, 6.5% of nursing home stays, and 9.1% of deaths. Without a definition of prehypertension, as we now have which has helped isolate the condition, these statistics at a minimum would have persisted under the radar without ever being noticed.
Yet another study published in 2001 in The Lancet (2001 Nov 17;358 (9294):1682-6) showed that within 4 years, 30% of individuals with pre-HTN (then refereed to as high normal blood pressure) would have converted from a state of pre-high blood pressure to hypertension.
Within 4 years, 30% of people with prehypertension would have converted to essential hypertension - Lancet Report (2001)
Altogether the establishment of a prehypertension definition describing what we now know as pre-HTN was an urgent medical opportunity to reduce, among other things, the prevalence of cardiovascular diseases in the population by preventing or delaying the progression of pre-high blood pressure to hypertension.
In the meantime, in view of a now established prehypertension definition, hypertension researchers have been equally seized with fully grasping causes and risk factors associated with pre-HTN.
Prehypertension Causes and Risk Factors
Credible peer reviewed studies have identified key risk factors which some have also loosely interpreted as causes of prehypertension. The following are frequently cited prehypertension risk factors cited in a variety of scientific studies
Body Mass Index and Waist Circumference
Body Mass Index (BMI) and Waist Circumference (WC) are highly regarded indicators or predictors of the development of pre-high blood pressure. They speak to concerns of being overweight and obese, themselves risk factors for not only prehypertension but also hypertension in general.
A 2014 study in the North American Journal of American Health Sciences (2014 Feb; 6(2): 89–95) sharing results of research on BMI and WC carried out in India, linked being overweight and obesity to a higher prevalence of pre-high blood pressure among the Punjabi community of between 18 and 50 years in Delhi.
The study discovered a notable association between BMI, fat percentage, and blood pressure both systolic blood pressure and diastolic blood pressure. Individuals having out of line BMI and WC had a higher chance of having high blood pressure compared to those with normal blood pressure.
To avoid prehypertension, it is critical to keep BMI and WC within acceptable parameters and this is achieved by maintaining the correct body weight for a person's age and height, for example. Found here are some tools to measure both BMI and WC.
Dyslipidemia
Dyslipidemia is a well known cause and recognized risk factor for prehypertension. It refers to having an abnormal amount of lipids (fat) in the blood. Typically a lipid count includes triglycerides, cholesterol and/or fat phospholipids measurement in a person's system.
Triglycerides are a type of fat that the body derives out of the conversation of calories. Cholesterol is fat-like substance also found in the cells of the body which can be good or bad cholesterol.
In the final analysis, dyslipidemia is very much linked to an individual's dietary patterns and is a risk factor for prehypertension in as much as it relates to a person's diet.
Apart from hypertension, dyslipidemia is also directly linked to coronary heart disease. As is the case with high blood pressure, dyslipidemia has no obvious symptoms and is only discovered or monitored through regular lab tests.
Fasting Plasma Glucose
Fasting Plasma Glucose (FPG) is known after a fasting plasma glucose test. It is an indicator used in the diagnosis of diabetes or pre-diabetes. Some 8 to 10 hours before the test no food nor drink must be ingested except for water. Fasting plasma glucose can be normal, impaired or diabetic.
Studies have used fasting plasma glucose as an important risk factor of prehypertension. A 2008 study published in the Indian Journal of Medical Research (2008 Dec;128(6):712-20) concluded that among other factors, impaired glucose tolerance or diabetes were strongly correlated to prehypertension and hypertension itself.
To arrive at this conclusion, the researchers involved 1112 people of 30 years of age or higher from the city of Lucknow, north India. Their plasma glucose and blood pressure measurements among other things were taken.
Prehypertension was highest at 36% in the group that was between 30 years and 39 years old. Individuals with prehypertension were found to be those with a frequency of glucose intolerance which was intermediate between normotensive and hypertensive participants.

Furthermore, another 2008 study published in the Japanese journal, Hypertension Research (2008 Jul;31(7):1323-30), found that impaired glucose tolerance and diabetes were determinants of pre-high blood pressure in females.
The participants in the study were 4706 Japanese males and 7 342 Japanese females aged between 18 to 90 years. Following their blood pressure measurement, they were further classified into normotensive, pre-HTN and hypertensive. Females (31.8%) had a lower prevalence of pre-high blood pressure than men (34.8%).
An interesting angle to the research findings was that fasting plasma glucose was an emphatic prehypertension risk factor in women than in men pointing to gender differences in prehypertension risk factors.
On a separate note, apart from confirming alcohol as a cause of pre-HTN particularly in men, the Japanese study also identified a family history of both parents with hypertension as a risk factor for pre-high blood pressure.
Smoking and Drinking
The role of smoking and drinking as a risk factor for prehypertension is still unresolved. While studies have shown that alcohol, for example, causes high blood pressure as we have shown here, the same cannot be said in harmony for pre-HTN.
For example, a 1998 study published in the journal Circulation (1998 May 26;97(20):2012-6) put forward evidence showing that tobacco cigarette smoke, through a complex biological mechanism, increased the level of low-density lipoprotein or LDL cholesterol. LDL cholesterol itself is part of dyslipidemia identified earlier as risk factor for prehypertension.
Yet on the other hand, another study also shared in a 1989 issue of the same journal, Circulation (1989 Nov;80(5):1309-12), absolved cigarette smoking of any role in increasing blood pressure. On average, the study found lower blood pressure in cigarette smokers compared to those who smoked.
Despite these apparent contradictions, for the most part literature has continued to list smoking and drinking as risk factors for prehypertension, perhaps as way of erring on the side of caution considering that there is evidence linking smoking and drinking to hypertension in general.
Summary of prehypertension predictors
- Body Mass Index and Waist Circumference (overweight/obesity)
- Dyslipidemia (poor diet)
- Fasting Plasma Glucose (impaired glucose tolerance and diabetes)
- Smoking and Drinking (still controversial)
- Alcohol (and being male, Japanese study)
- Family history (both parents with hypertension)
- Being female (and having impaired glucose intolerance)
Under these circumstances, one of the most frequently asked questions is how then to treat prehypertension with or without drugs.
Prehypertension Treatment and Drugs
While its accepted that pre-high blood pressure must be treated due to its known progression to hypertension, one of the burning questions in hypertension science and among ordinary folks is whether prehypertension treatment should be with lifestyle changes or with medications.
Lifestyle Modifications
A 2012 review in the journal, Vascular Health and Risk Management (2012; 8: 613–619), favored the use of lifestyle modifications in treating prehypertension. The researchers noted that while high blood pressure medications were effective in reducing blood pressure, treating everyone with pre-high blood pressure would turn no less than 25 million people, in the case of the United States, into patienthood. Furthermore, such a development would also put an unbearable burden on the health care system in any society.
The review recommends that prehypertension must be treated using lifestyle modifications particularly regular exercise. The advantages of exercises in treating pre-HTN, apart from little or no side effects, include a address on multiple physiological systems which is beneficial to overall health and well being of the individual.
In addition, the researchers recommend that regular exercise should be inculcated in children and form part of daily therapy to prevent a variety of health problems and not only hypertension.
The 2001 Lancet study that we refereed to earlier recommends that emphasis should be put on weight control in order to prevent progression of pre-high blood pressure to hypertension.
Weight control directly deals with Body Mass Index and Waist Circumference that were identified as important risk factors for prehypertension. According to the Lancet study, a 5% gain in weight was shown to increase the odds of hypertension by some 20 to 30%.
Weight control is very much linked to diet. Eating healthy is a necessary measure to be taken as part of treating prehypertension. In this regard, we have written extensively on the benefits of foods such as celery and beets among others in lowering blood pressure. Use of scientifically proven to be effective blood pressure herbs is also worth considering.

Summary of lifestyle modifications that can be considered in treating prehypertension
- Daily exercise
- Weight control/Weight loss
- Eating healthy
- Use of scientifically proven herbs
- Normal Blood Pressure Monitoring (every 2 years)
- Quitting smoking
- Managing alcohol consumption
On the other hand, some have also considered the use of pharmacological drugs to treat prehypertension, the overall outlook has not been good.
Treatment using Drugs
In general physicians concede that lifestyle modifications should be the first line of treatment for pre-high blood pressure. Be that as it may, a 2006 study published in the New England Journal of Medicine (2006 Apr 20;354(16):1685-97) demonstrated the feasibility of treating prehypertension using drugs.
The study, entitled Feasibility of treating prehypertension with an angiotensin-receptor blocker, noted that over a period of four years drugs prevented the progression of prehypertension to stage 1 hypertension as is usually the case. During the study, the researchers used candesartan, a hypertension drug in the class of angiotensin receptor blockers (ARBs).
Despite such supportive and glorious scientific evidence, there remains a lingering reluctance among physicians to recommend the use of drugs to treat prehypertension.
The argument has been that if late intervention using drugs when hypertension has developed is as effective as early intervention when it is still pre-HTN, as some studies have shown, in order to minimise patienthood burden and other associated problems such as drug side effects one is better off staying away from drug treatment at this stage.
All things considered it becomes the call of the patient working with their physician whether or not to use pharmacological drugs in treating prehypertension.
Prehypertension during Pregnancy
While there has been increased focus on gestational hypertension, hypertension researchers have also increasingly considered prehypertension during pregnancy.
Until recent times there had been limited studies into the effect of prehypertension during pregnancy. That information still remains largely limited.
One of the most important studies to flag possible risks associated with prehypertension during pregnancy was published in 2016 in the journal Hypertension (2016 Mar;67(3):640-6). The conclusion of the study, involving 157 446 women, is that prehypertension occurring in late pregnancy is linked to increased risks of small-for-gestational-age (SGA) birth and stillbirth.
In a similar fashion as we explain in our article on high blood pressure in pregnancy, the study described how pre-high blood pressure impaired the maternal perfusion of the placenta. Placenta perfusion simply refers to the compromise to the placenta resulting in reduced flow of oxygen, blood and nutrients from mother to baby in the womb. This ends in SGA and possible still birth.
A 2017 report in The Journal of Maternal-Fetal & Neonatal Medicine (2017 Sep 12:1-5) gave further support to the Hypertension journal findings. The study made a comparison of the effects of prehypertension during pregnancy in its early days, that is less than 20 weeks of pregnancy and during its later days greater than 20 week of pregnancy.
The study involving 377 people concluded that early pre-high blood pressure in pregnancy increased the risk of dangerous child birth outcomes. On the other hand prehypertension occurring later on during pregnancy beyond 20 weeks increased risk of pregnancy-related hypertension.
There is yet another study whose results were equally insightful in respect of pre-high blood pressure and pregnancy. A 2015 report of the study published in the Journal of Hypertension (2015 Sep;33(9):1860-7) involving over 7800 women, linked prehypertension in pregnancy to gestational diabetes mellitus (GDM) and pre-eclampsia/eclampsia. GDM is glucose intolerance in pregnancy.
The study observed that pregnant women with pre-HTN had a 1,20 more likely chance to develop gestational diabetes mellitus compared to pregnant women with normal blood pressure. They also had a 2.65 chance of suffering from pre-eclampsia/eclampsia compared to their normotensive counterparts.
Considering what has come out of these studies, there is indeed convincing evidence suggesting that prehypertension during pregnancy should not be ignored as benign.

summary of possible complications of prehypertension during pregnancy
- Small-for-gestational-age (SGA) birth
- Still birth
- Increased risk of pregnancy-related hypertension
- Increased risk of dangerous obstetrical (baby birth) outcomes
- Gestational diabetes mellitus (GDM)
- Pre-eclampsia/eclampsia
[Last updated: 01 November 2017]

|
|
Alcohol and Blood Pressure |
Return To Hypertension Guidelines from Prehypertension
Return To Hypertension Home from Prehypertension
Disclaimer
Information contained on this website is not meant to replace your doctor's advice.
(c) All Rights Reserved. 2010-2018